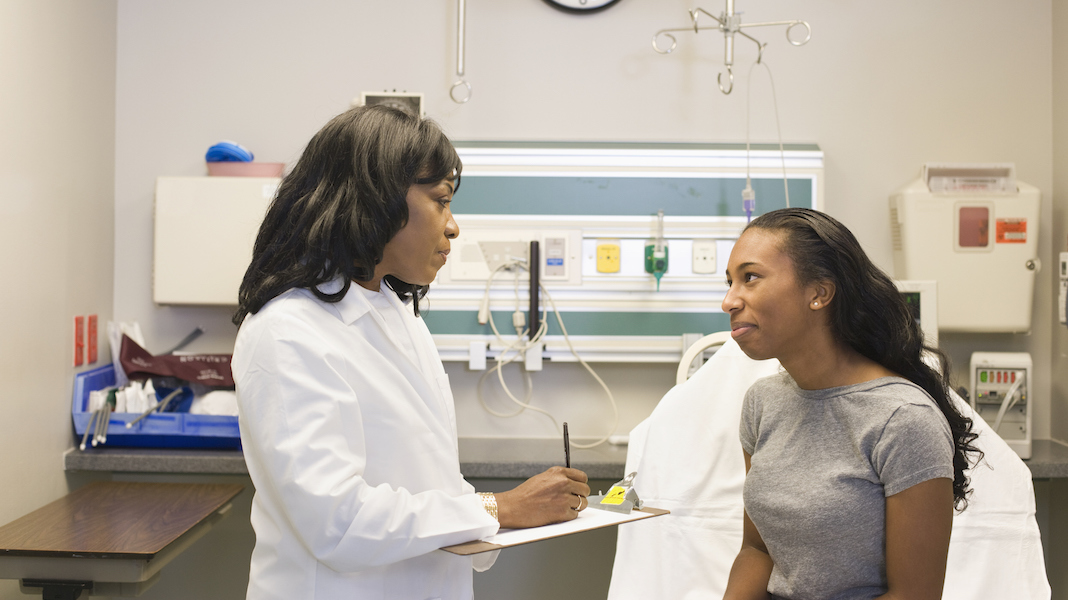
Gettyimages.com/Doctor talking to patient in hospital
Have you ever had someone explain the benefits and conditions of a health insurance plan to you before, and wanted to stop them so they could explain one confusing term, but before you had the chance, they’d already said five other words you didn’t know? At that point, you know that you just need to make a mental note of the things they said and look them up in a dictionary later or else this conversation will never end. This is a pretty common experience and that’s a shame because understanding the jargon in your health insurance plan is rather important. We’re here to help, and nobody even has to know that you ever needed our help. Here are health insurance terms we’re all just pretending to understand.

Image Source: Shutterstock
Accumulation period
If your claims adjustor ever tells you he won’t pay out your claim because you’re still in your accumulation period, all he means is that you haven’t yet met your deductible. If you’re still in your accumulation period, even claims that would normally be covered by your insurance won’t yet be covered until you meet your deductible.